April Calendar PDF: A Comprehensive Guide
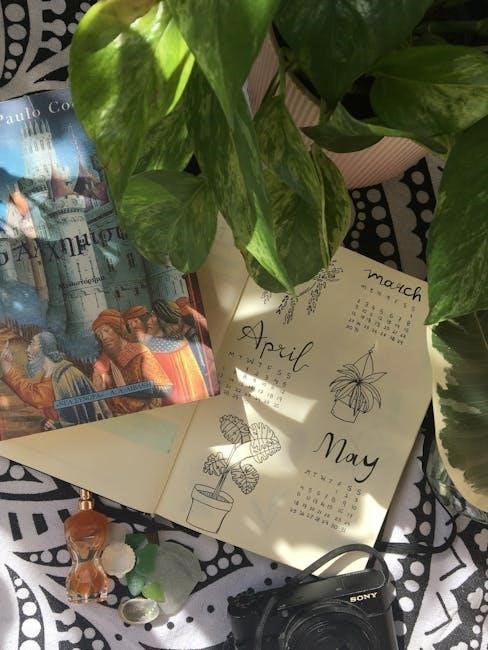
Discover a wealth of free, downloadable April 2024 calendar PDFs from sites like EntheosWeb and Dishcuss, offering diverse layouts for seamless organization.

What is an April Calendar PDF?
An April Calendar PDF is a digital document, specifically in Portable Document Format, designed to display the days, weeks, and events of April in a structured manner. These calendars, readily available for free download from websites like EntheosWeb.com and Dishcuss.com, offer a convenient and universally accessible way to plan and organize the month.
Unlike traditional paper calendars, a PDF version allows for easy printing, digital storage, and often, customization. They come in various layouts – monthly, weekly, or daily – catering to different planning preferences. The visual examples found online showcase diverse designs, from simple and functional to more aesthetically pleasing options, including themed calendars.
Why Use a Printable April Calendar?
Printable April calendars offer a tangible planning experience, distinct from digital alternatives. They allow for visual overview of the month, facilitating better time management and event tracking. Downloading PDFs from sources like EntheosWeb and Dishcuss provides readily available, customizable templates.
The act of physically writing appointments and tasks can enhance memory retention. Printable calendars also eliminate digital distractions, promoting focused planning. Furthermore, they’re ideal for shared spaces – kitchens, offices – ensuring everyone stays informed; The convenience of printing allows for personalized sizes and layouts, adapting to individual needs and preferences.
Benefits of Using a PDF Format
PDFs ensure your April calendar appears consistently across all devices and operating systems, preserving formatting from sites like EntheosWeb and Dishcuss. This universal compatibility is a key advantage. They are easily downloadable and shareable, making collaboration simple.
PDFs are also relatively secure, preventing unintended alterations to your carefully planned schedule. While some PDFs allow editing with tools like Adobe Acrobat Reader, many offer protection against accidental changes. Their compact file size facilitates easy storage and quick access, streamlining your organizational process.
Types of April Calendar PDFs Available
A diverse range of April calendar PDFs caters to varied preferences. Standard monthly calendars provide a traditional overview, while weekly layouts offer more detailed scheduling. Daily planner calendars are ideal for meticulous time management.
Beyond functionality, themed calendars – such as floral or Easter designs – add a personal touch. Resources like EntheosWeb and Dishcuss showcase these options. Users can find calendars prioritizing aesthetics alongside practicality, ensuring a visually appealing and organized April. The availability is broad, fitting diverse needs.

Standard Monthly Calendar
The classic April calendar PDF typically presents a full month on a single page, showcasing all dates at a glance. This format is ideal for noting key appointments and deadlines without excessive detail. EntheosWeb and Dishcuss both offer variations of this standard layout, often with clean, minimalist designs.
These calendars prioritize overview and simplicity, making them perfect for wall display or quick reference. They are a foundational choice for basic scheduling needs, providing a clear visual representation of April’s structure.
Weekly Calendar Layouts
Weekly April calendar PDFs break down the month into individual weeks, offering more space for detailed planning. These layouts, available from resources like EntheosWeb and Dishcuss, typically display Monday to Sunday, allowing for specific daily task allocation.
This format is beneficial for those who prefer a more granular approach to scheduling, enabling them to visualize their week at a glance. The increased space accommodates notes, to-do lists, and reminders, promoting better time management and organization throughout April.
Daily Planner Calendars

For meticulous scheduling, daily planner April calendar PDFs provide the most detailed organization. These layouts dedicate a full page (or more) to each day of April, allowing ample space for hourly breakdowns and comprehensive task lists.
Resources like EntheosWeb and Dishcuss may offer these, catering to individuals who thrive on detailed planning. This format is ideal for managing appointments, projects, and personal commitments with precision, ensuring no detail is overlooked throughout the month of April.
Themed April Calendars (Floral, Easter, etc.)
Elevate your planning with visually appealing themed April calendar PDFs! Many websites offer calendars incorporating seasonal designs like blooming florals or festive Easter imagery. These calendars blend functionality with aesthetics, making planning a more enjoyable experience.
EntheosWeb and similar platforms frequently showcase these options, providing a delightful touch to your daily organization. Themed calendars can brighten your workspace and add a personal flair to your April schedule, making it both practical and visually stimulating.
Where to Find Free April Calendar PDFs
Numerous online resources offer free April calendar PDFs for download. EntheosWeb.com stands out as a prominent source, providing a variety of printable calendar designs to suit different preferences. Dishcuss.com also presents options, alongside other websites dedicated to free printable resources.
A quick online search will reveal a plethora of choices, ranging from simple monthly layouts to more elaborate designs. These platforms generally offer calendars in PDF format, ensuring easy access and compatibility across various devices. Explore these sites to find the perfect calendar!
EntheosWeb.com
EntheosWeb.com is a valuable resource for obtaining free April 2024 printable calendars in PDF format. The site offers a selection of visually appealing calendar designs, readily available for download. Users can find calendars suitable for various organizational needs, from basic monthly overviews to more detailed planning layouts.
Their offerings include Pinterest-inspired pin designs, showcasing sample calendars. EntheosWeb provides a convenient and accessible platform for individuals seeking free, high-quality April calendars to enhance their scheduling and productivity. It’s a great starting point for your search!
Dishcuss.com
Dishcuss.com presents a diverse collection of April 2024 calendar options, available as free PDF downloads. The platform features calendars with varying aesthetic styles, including designs incorporating red and white color schemes and icon-based layouts. Users can explore options like “Sample Calendar 2024” and “Month 7 Calendar” to find a suitable template.
Dishcuss provides a visually-driven experience, with thumbnails showcasing calendar designs. It’s a useful resource for those seeking unique and readily printable April calendars to aid in personal or professional organization. The site offers a quick way to access calendar templates.
Other Online Resources for Free Calendars
Beyond EntheosWeb and Dishcuss, numerous online platforms offer free April 2024 calendar PDFs. A broad Yandex image search reveals a multitude of options, though specific site details require further investigation. Many websites specialize in printable templates, including calendars, catering to diverse organizational needs.
Exploring these resources often involves navigating through various designs and formats. Users can typically filter by style, layout (monthly, weekly, daily), and theme. Remember to verify download safety and file integrity before opening any PDF from unfamiliar sources. A little searching yields plentiful choices!

Customizing Your April Calendar PDF
Personalize your April calendar PDF to maximize its utility! After downloading, readily add personal events, appointments, and reminders. Utilize PDF editing software – like Adobe Acrobat Reader or alternatives – to directly input text. Enhance organization by employing highlighting and color-coding for different event categories.
Consider adding notes, stickers, or even images to make your calendar visually appealing and uniquely yours. This customization transforms a generic template into a powerful, personalized planning tool, perfectly tailored to your specific needs and schedule.
Adding Personal Events and Appointments
Seamlessly integrate your life into your April calendar PDF! After downloading a template, begin by directly adding personal events – birthdays, anniversaries, or social gatherings. Don’t forget important appointments, like doctor visits or meetings. Utilize the PDF’s text editing features to clearly label each entry with date, time, and a brief description.
Remember to include recurring events for convenience. A well-populated calendar, reflecting your commitments, becomes an invaluable tool for time management and ensuring nothing slips through the cracks throughout April.
Using Highlighting and Color-Coding
Maximize your April calendar PDF’s effectiveness with strategic highlighting and color-coding! Assign distinct colors to different event categories – work, personal, family, or health. This visual cue instantly differentiates commitments at a glance. Utilize highlighting to emphasize crucial deadlines or appointments requiring immediate attention.
Consider a key or legend to clarify your color scheme. This simple technique transforms a standard calendar into a dynamic, easily navigable overview of your April schedule, boosting productivity and reducing the risk of overlooked obligations.
Printing Options and Paper Size
When printing your April calendar PDF, consider your needs. Standard US Letter (8.5 x 11 inches) is common, but A4 paper (210 x 297 mm) is also suitable. Check your printer settings for optimal scaling – ensure the calendar fits the page without cropping.
Experiment with grayscale or color printing based on your preference and ink availability. For durability, print on heavier weight paper. Many PDFs offer options for multiple calendars per page, ideal for compact overviews. Preview the print before finalizing to avoid wasted paper!
Software for Opening and Editing PDF Calendars
Adobe Acrobat Reader is the gold standard for viewing PDFs, offering reliable performance and accessibility features. However, several alternatives exist! Foxit Reader and Sumatra PDF are lightweight and fast options. For basic editing – adding text or highlighting – consider PDFescape or Smallpdf online.
More advanced editing, like changing calendar content, often requires a paid Adobe Acrobat subscription. Ensure your chosen software supports the PDF version of your April calendar for seamless viewing and functionality.
Adobe Acrobat Reader

Adobe Acrobat Reader remains the most widely used software for opening and interacting with PDF April calendars. It’s a free, reliable tool available for Windows and macOS, ensuring consistent viewing across platforms. Beyond simple viewing, it offers features like digital signatures and form filling.
While basic functionality is free, advanced editing capabilities require a paid subscription to Adobe Acrobat Pro. However, for simply viewing, printing, and annotating your April calendar PDF, the Reader version is perfectly sufficient and readily accessible to most users.
Alternative PDF Readers
Fortunately, several excellent alternatives to Adobe Acrobat Reader exist for viewing April calendar PDFs. Foxit Reader is a popular choice, offering a lightweight and fast experience with similar features. SumatraPDF is another free option, known for its minimal design and portability – ideal for quick access.
These alternatives generally support basic PDF functions like printing and searching, ensuring you can effectively utilize your downloaded April calendars. Choosing an alternative often depends on personal preference and specific feature requirements, providing flexibility beyond Adobe’s ecosystem.
Basic PDF Editing Tools
While full-scale PDF editing often requires paid software, several tools allow basic modifications to your April calendar PDFs. Adobe Acrobat Reader DC itself offers features like adding text comments and highlighting important dates. Online PDF editors, such as Smallpdf or iLovePDF, provide browser-based options for simple tasks like merging or splitting files.
These tools are useful for adding personal notes or reminders directly onto your calendar. However, remember that free tools may have limitations on editing capabilities, so complex changes might necessitate more robust software.
Tips for Effective Calendar Use
To maximize the benefits of your April calendar PDF, prioritize tasks by marking deadlines and important events with distinct colors. Utilize highlighting to draw attention to key appointments or reminders. Implement time blocking techniques, scheduling specific blocks for focused work or dedicated activities.
Set reminders – digital or physical – to ensure you never miss a crucial date. Regularly review your calendar, ideally daily, to stay organized and proactive. A well-used calendar transforms from a simple date tracker into a powerful productivity tool.
Prioritizing Tasks
Effectively using your April calendar PDF begins with task prioritization. Identify critical deadlines and appointments, marking them prominently with color-coding. Distinguish between urgent and important tasks; focus on high-impact activities first. Break down larger projects into smaller, manageable steps and schedule them accordingly.
Utilize the calendar to allocate specific time slots for each task, preventing overwhelm. Regularly reassess priorities as new commitments arise. A prioritized calendar isn’t just about scheduling; it’s about focused action and achieving goals.
Setting Reminders
Maximize your April calendar PDF’s utility by integrating reminders. Leverage the digital features of your PDF reader – many allow direct reminder settings linked to your device. Alternatively, manually note reminders alongside events within the calendar itself. Consider setting multiple reminders for crucial deadlines, ensuring ample preparation time.
Don’t rely solely on the calendar; synchronize it with your preferred task management apps. Regularly review upcoming events and reminders to stay proactive. Effective reminders transform your calendar from a passive schedule into an active productivity tool.
Time Blocking Techniques
Enhance productivity with time blocking, utilizing your April calendar PDF to schedule dedicated blocks for specific tasks. Allocate fixed time slots for work, appointments, and even leisure, treating each block as a non-negotiable commitment. Visually delineate these blocks using color-coding within your PDF for easy identification.
Prioritize deep work by scheduling uninterrupted blocks. Buffer time between blocks for transitions and unexpected delays. Regularly review and adjust your time blocks based on actual task completion rates, optimizing your schedule for maximum efficiency.
April 2024 Specific Events & Holidays to Include
Ensure your April 2024 calendar PDF incorporates key dates for comprehensive planning. Mark Easter (date varies), a significant holiday often requiring travel or family gatherings. Don’t forget April Fool’s Day, a lighthearted occasion for fun. Highlight Earth Day, prompting environmental awareness and potential activities.
Add any personal events coinciding with these dates. Utilize color-coding to differentiate between holidays, appointments, and personal commitments within your PDF. Regularly check for accuracy, ensuring a well-organized and informative April calendar.
Easter (Date Specific)
Easter’s date fluctuates annually, making it crucial to verify the specific date for April 2024 when populating your calendar PDF. Typically, Easter falls between March 22nd and April 25th. In 2024, Easter is on March 31st, but planning often extends into early April.
Mark Easter Sunday and any related events – church services, family brunches, or egg hunts – directly onto your April calendar PDF. Consider adding reminders leading up to the holiday for preparations. Utilize color-coding to visually distinguish Easter-related events from other appointments.
April Fool’s Day
April Fool’s Day, observed annually on April 1st, is a day for lighthearted pranks and playful jokes. Integrate a reminder into your April calendar PDF to anticipate potential trickery or to plan a harmless prank of your own! Consider noting it with a playful icon or color to easily identify the date;
While primarily a day for fun, it’s wise to remain mindful of work commitments and important appointments. Ensure any planned pranks don’t disrupt crucial tasks. Your April calendar PDF can serve as a reminder to balance amusement with responsibility on this quirky holiday.
Earth Day
Earth Day, falling on April 22nd, is a crucial date dedicated to environmental awareness and action. Utilize your April calendar PDF to schedule eco-friendly activities, such as volunteering for a cleanup, planting trees, or simply reducing your carbon footprint. Mark the date prominently with a green icon or color-coding to emphasize its importance.
Beyond a simple reminder, your calendar can house specific plans – a recycling drop-off, a nature walk, or research into sustainable practices. Integrating Earth Day into your schedule via a PDF calendar fosters a proactive approach to environmental responsibility throughout the month.
Downloading and Saving April Calendar PDFs
Upon finding your desired April calendar PDF from resources like EntheosWeb or Dishcuss, ensure a smooth download process. Select “Save” rather than “Save As” to utilize default folder settings, or choose a dedicated “Calendars” folder for organization. Employ clear file naming conventions – “April2024Calendar_Weekly” or “April2024_Floral” – for easy identification.
Regularly back up these files to a cloud service or external drive to prevent data loss. Consider creating duplicate copies for redundancy. Consistent organization and backups safeguard your customized April calendar, ensuring accessibility and peace of mind throughout the month.
File Naming Conventions
Establishing consistent file naming conventions is crucial for efficient April calendar PDF management. Incorporate the month and year – “April2024” – as a prefix for immediate identification. Add descriptors indicating the calendar’s layout, such as “_Weekly,” “_Monthly,” or “_Daily.” For themed calendars, include keywords like “_Floral” or “_Easter.”
Avoid spaces and special characters; use underscores (_) instead. Maintain a uniform structure across all files. Example: “April2024_Monthly_Floral.pdf”. This systematic approach streamlines searching and organization, saving valuable time when accessing your preferred April calendar.

Organizing Your Calendar Files
Effective organization of your April calendar PDFs is key to productivity. Create a dedicated folder – for example, “Calendars” or “April_Calendars” – within your document storage system. Consider subfolders based on calendar type: “Monthly,” “Weekly,” “Daily,” and “Themed.”
Consistently save downloaded PDFs into their respective folders immediately. Regularly review and delete duplicates. Utilize cloud storage services like Google Drive or Dropbox for accessibility and backup. A well-structured file system ensures quick retrieval of your desired April calendar, maximizing efficiency and minimizing frustration.
Backing Up Your Calendars
Protecting your meticulously planned April calendar PDFs is crucial. Regularly back up your calendar files to prevent data loss due to technical issues or accidental deletion. Utilize cloud storage solutions like Google Drive, Dropbox, or OneDrive for automatic backups.
Alternatively, copy your calendar folder to an external hard drive or USB flash drive. Implement a backup schedule – weekly or monthly – to ensure your data remains current; Consider a redundant backup strategy, using multiple backup methods for enhanced security and peace of mind.
Troubleshooting Common PDF Issues
Encountering problems with your April calendar PDFs? If a PDF won’t open, ensure you have a compatible PDF reader like Adobe Acrobat Reader installed and updated. Check file associations to confirm PDFs are linked to the correct program.
For printing issues, verify your printer is connected and has sufficient ink or toner. If editing is restricted, the PDF may be secured; look for options to request permission. Try a different PDF reader if one fails. Restarting your computer can often resolve temporary glitches.
PDF Won’t Open
Facing difficulty opening your April calendar PDF? First, confirm you have a reliable PDF reader installed, such as Adobe Acrobat Reader, and that it’s the latest version. Ensure the file hasn’t been corrupted during download – try downloading it again from the source.
Check if the file association for PDFs is correctly linked to your chosen reader in your operating system settings. A damaged PDF reader installation might also be the culprit; try reinstalling it. Finally, a very large or complex PDF could cause issues on older systems.
Printing Problems
Experiencing issues printing your April calendar PDF? Verify your printer is correctly connected and has sufficient ink or toner. Ensure the correct printer is selected within the print dialog box of your PDF reader. Check the page scaling option; selecting “Fit” or “Shrink to Fit” can resolve cropping issues.
Confirm your paper size settings in both the PDF reader and your printer settings match the paper loaded in the tray. A corrupted printer driver could also be the cause – try updating or reinstalling it. Lastly, test printing a different PDF to isolate the problem.
Editing Restrictions
Many April calendar PDFs are designed as static documents, meaning direct editing of text and graphics within standard PDF readers like Adobe Acrobat Reader may be limited; This is often intentional, preserving the calendar’s formatting. However, some PDFs may allow filling in form fields or adding text annotations.
For extensive edits, consider using a full-featured PDF editor, though these often require a paid subscription. Alternatively, you could print the calendar and manually write in your appointments. Understanding these restrictions helps manage expectations when personalizing your chosen April calendar PDF.
Accessibility Features in PDF Calendars
Modern April calendar PDFs increasingly incorporate accessibility features for diverse users. Crucially, screen reader compatibility allows visually impaired individuals to navigate and interpret calendar content effectively. Adjustable font sizes cater to those with visual preferences or needs, enhancing readability.
Furthermore, thoughtful design includes color contrast options, ensuring information is discernible for users with color blindness. Well-structured PDFs with tagged content improve navigation for assistive technologies. These features promote inclusivity, making April calendars usable by a wider audience.
Screen Reader Compatibility
Ensuring April calendar PDFs are screen reader compatible is paramount for accessibility. Properly tagged PDFs allow screen readers to interpret the document’s structure, conveying dates, events, and notes to visually impaired users. This involves defining headings, lists, and table structures accurately.

Alternative text descriptions for images, like calendar graphics, are also vital. A well-constructed PDF enables seamless navigation using keyboard commands. Testing with various screen readers—like JAWS or NVDA—confirms functionality. Ultimately, compatibility empowers all users to effectively manage their April schedules.
Adjustable Font Sizes
A key accessibility feature of April calendar PDFs is adjustable font sizing. Users with visual impairments or preferences for larger text benefit greatly from this capability. Reflowable text, adapting to the screen size, enhances readability. Many PDF readers, including Adobe Acrobat Reader, offer zoom functions and font size controls.
This allows individuals to customize the calendar’s appearance for optimal comfort. Ensuring the PDF isn’t image-based, but utilizes actual text, is crucial for resizing to work effectively. Prioritizing accessibility means catering to diverse visual needs.
Color Contrast Options
Effective April calendar PDFs prioritize color contrast for improved readability, especially for users with visual impairments. High contrast between text and background colors – like black text on a white background, or vice versa – significantly reduces eye strain. Some PDF creators offer pre-set high contrast themes.

Alternatively, users can often adjust color settings within their PDF reader. Consider avoiding color combinations that are difficult to distinguish, such as light blue and yellow. Accessibility guidelines recommend a contrast ratio of at least 4.5:1 for normal text and 3:1 for large text.